Prevalence of Pelvic Organ Prolapse
According to Yale Medicine, 25% of women over the age of 18 suffer from some type of pelvic floor disorder. One of these common issues is pelvic organ prolapse or POP. Pelvic organ prolapse is a condition where one or more of the pelvic organs, including rectum, bladder, uterus or urethra descends and pushes into the vaginal wall.
At first diagnosis, prolapse can be very scary. Many women may wonder if their internal organs are going to just right out of them! While sever cases can see the vaginal wall protruding outside the body, in majority of cases the organ stays within the body and can be treated conservatively with pelvic floor physical therapy.
In this blog we are going to review POP stages, risk factors, symptoms, and how physical therapy can be an effective way to manage and overcome your prolapse.
What is prolapse?

As stated, prolapse is when one or more of the pelvic
organs pushes into the vaginal wall and descends into the
pelvic cavity. (It also important to note that a rectal
prolapse can also occur, which is when the rectums descends
and protrudes towards the anal opening, however we are going
to focus on vaginal prolapse in this blog.) The most common
way to diagnosis and grade a prolapse is with the
POP-Q. The POP-Q quantifies the severity of the prolapse
by measuring the most distal portion of the prolapse
in relation to the hymen, or vaginal opening, while
the patient is straining (think: bearing down in
the way you would when having a bowel movement).
The POP-Q ranks 0 as no prolapse present while a grade
4 is when the majority of the vaginal wall is outside
the vaginal opening.
However, it is super important to note that the research has shown that prolapse grade does NOT correspond with severity of symptoms. I think this is so so encouraging for patients because it means that the grade of their prolapse doesn’t determine what they can or can’t do! It means you can have a “severe” prolapse but still feel great, workout the way you want to and live your life to the fullest!
Risk Factors for Prolapse
The most common risk factor for prolapse is pregnancy due to the increased pressure & demand on the pelvic floor muscles & connective tissue. Prolonged pushing during childbirth, repeated straining during bowel movements or heavy lifting can also contribute to prolapse.
Symptoms of Prolapse
Symptoms of prolapse include a feeling of pressure, bulging or heaviness in the vagina or pelvis, a visible bulge, bleeding, low back ache and difficulty emptying the bowels or bladder. These symptoms can range from mild to severe and can fluctuate in when they are felt such as at the end of the day.
How Pelvic Floor Physical Therapy Can Help
Pelvic floor physical therapy is an effective treatment method for prolapse and majority of cases can be treated successfully. While the symptoms of prolapse are typically confined to the pelvis, the rest of the body has a tremendous influence on prolapse symptoms and support of the pelvic organs. The way that we breathe, sit, stand, engage our core, pick up our kids, lift weights and manage our stress impacts our pelvic floor! Seeing a knowledgeable pelvic floor physical therapist who looks not only at the pelvic floor, but the rest of the body will be able to help you correct your movement patterns, strengthen your pelvic floor, hips & core in order to decrease your symptoms!
What does pelvic floor physical therapy for prolapse look like?
If you aren’t familiar at all with pelvic floor physical therapy, check out our blog “Pelvic Floor Physical Therapy: Everything You Need to Know”
During your first session your pelvic floor physical therapist will assess your whole-body movement, core & hip strength during functional movements, your breathing pattern, pelvic alignment & assess the strength & pliability of your pelvic floor muscles. After areas for improvement are identified your pelvic floor physical therapist will start to create a program unique to you.
Strengthening
While each person is different, in my experience most people with prolapse need to work on some form of strengthening. This may include Kegels, as often times doing Kegels can help relieve prolapse symptoms and build back strength in the pelvic floor muscles, especially after childbirth. However, the core, glutes, hamstrings and quads also play a huge role in supporting our pelvis and therefore the pelvic organs so it is imperative that these muscles are being strengthened as well. Below are two great exercises to start working on the glutes and core.
Functional Progression 1
Marching Bridge with Pelvic Floor Engagement
*If you feel any increase in symptoms doing these exercises please do not continue performing and seek out an evaluation from a pelvic floor physical therapist.
I also want to point out that lifting too heavy with improper breathing mechanics can contribute to prolapse, but this doesn’t mean exercise should be avoided all together. In fact, many clients report and increase in symptoms when they DON’T exercise. The secret is not so much in whatyou’re doing but how you are doing it. This is where working with a pelvic floor physical therapist who knows exercise (and the type of exercise you do) can help you learn how to safely exercise and utilize strength training in order to overcome prolapse.
Breathing
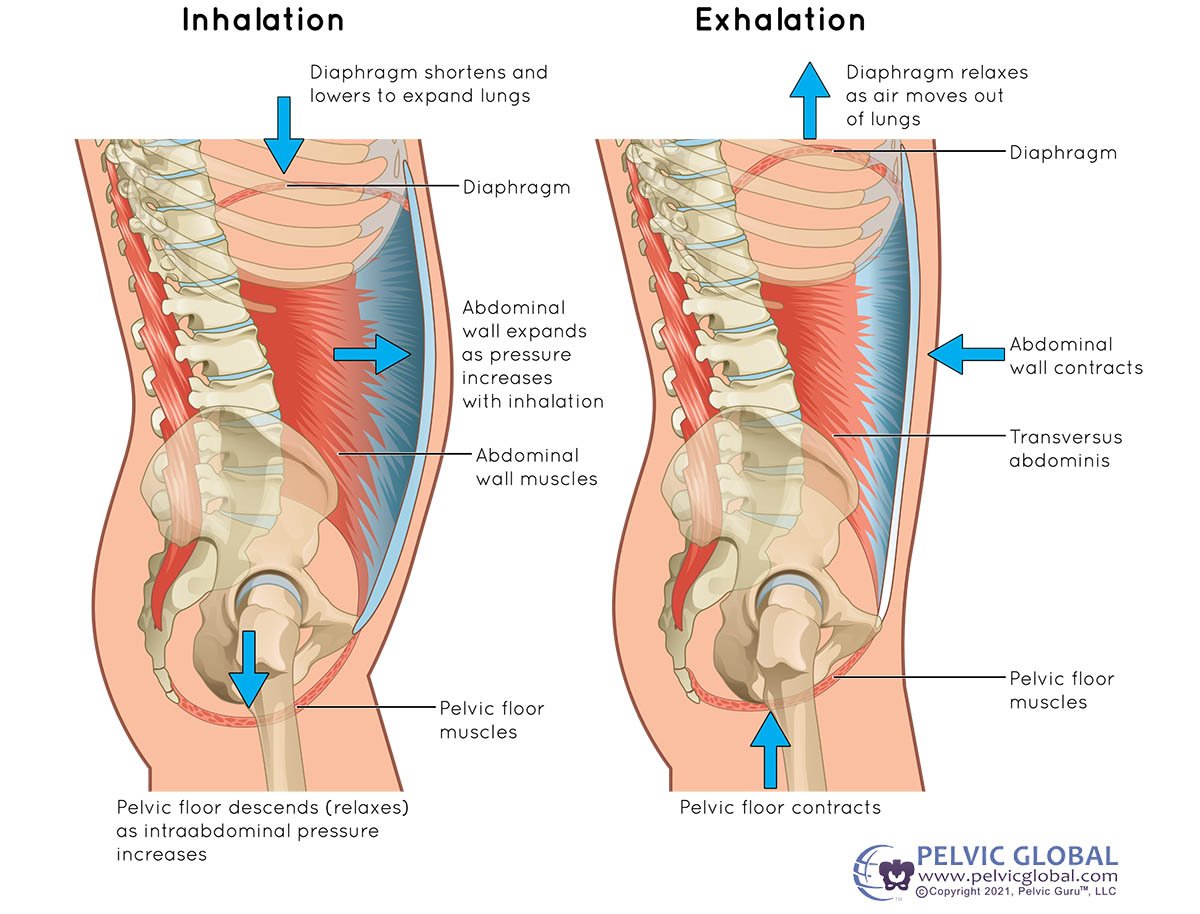
The next part of pelvic floor physical therapy that
is incredibly important is working on and improving
your breathing mechanics. If you are someone who is always
breathing really shallow, using your neck & shoulders,
this is likely negatively impacting your pelvic floor.
Alternately you may be keeping your neck relaxed but only
breathing into your belly. Both of these are problematic,
(for different reasons) and while I won’t go into detail
about why in this blog, it is important to correct
breathing to what we call a 360 pattern which utilizes
the back, lateral rib cage and belly all evenly. When the
back & rib cage expand in addition to the belly it allows
for even distribution of intraabdominal pressure
(a normal thing we need during an inhale) and helps
not to put too much pressure downward on our pelvic
organs. Adopting this breathing pattern first at
rest, then during exercise and under fatigue is
imperative to managing prolapse symptoms. Below
are two breathing exercises I utilize with my clients:
Lateral Rib Cage Breathing with a Band
Lifestyle management
Another important part of treating prolapse and an aspect many MDs unfortunately don’t focus on is lifestyle management. This includes things such as stress and schedule management and healthy bowel routines. It is no secret prolonged stress isn’t good for us, but many people don’t always think about how their emotional or mental stress impacts them physically. Often times I will start to work with moms as early as 3 weeks postpartum. I’ve been able to help moms to manage and decrease their prolapse symptoms to where they are feeling awesome by the time they go back to work, however once they return to work and their schedule changes they tend to see an increase in symptoms. This is usually because it’s a stressful transition (and understandably so) but realizing this, giving yourself grace and finding healthy ways to manage stress are so important.

A physical therapist can also help you create
a healthy bowel routine so you can avoid straining
and potentially making your prolapse worse. This includes
discussing diet & hydration, healthy toileting
posture (think: squatty potty!) and teach you
techniques such as splinting; which is using your
finger or a device to put pressure on the perinium
or rectum during bowel movements to provide extra
support to the pelvic organs.
“Image used with permission from Pelvic Guru®, LLC www.pelvicglobal.com”
So, while pelvic organ prolapse can be a scary diagnosis, physical therapy can an extremely effective tool in overcoming it! A pelvic floor physical therapist will be able to help you with strengthening, breathing & movement and lifestyle factors that play a role in prolapse symptoms.
If you think you may have prolapse, contact us, today in order to talk to member of our team to see how we can help you!
Sources:
Yale Medicine
NIH
AAFP